
With billing, coding and claims processing as our specialty, we offer a complete business process solution for your medical practice that is optimized, efficient, smart, and make a good business sense. This includes, but not limited to,

Credentialing Services:
Our service includes provider credentialing, contracting with the insurance Companies, and re-credentialing. We work with all specialties and assist with enrollment in all insurance networks (Medicare, Medicaid, and Commercial Insurance).
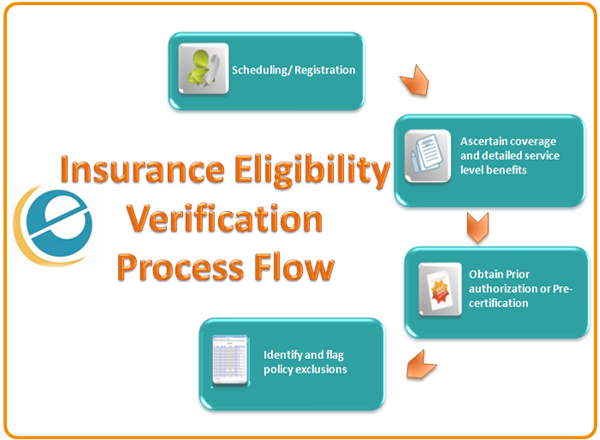
Insurance Eligibility Verification:
We verify each and every Patient’s insurance coverage before they are seen by the Doctor to reduce the denials and maximize collections. Daily alerts/mails are sent to the Physician with eligibility verification details including deductible, co-pay information, coverage date, etc. before the patient’s appointment.
Coding & Data Entry:
We customize our billing service to meet your individual needs. We are capable to use your existing billing system, EMR and EHR. If your billing systems are installed on your computers in your office, we are capable of remotely accessing your systems with our robust and secured technologies. There are also options for utilizing fax and secure cloud storage services.

File Claims – Most claims are filed electronically and only a few will go on paper where necessary because of the limitations of a given insurance carrier.

Payments Posting :
We will establish electronic payments for you so that your payments are directly deposited into your designated bank account. We will collect all payments from the insurance carriers and apply them to your submitted claims.
Receivables Follow Up: Claims are continually worked on, resubmitted and processed until payment is received. Proactive follow up starts from the 21st day of the initial claim submission.
Denial Management and Revenue Recovery:
Unpaid or underpaid receivables are followed up, reasons for non-payments are clarified and corrective measures are taken to recover the outstanding unpaid balances. All denials are worked on with relentless follow up accompanied by all necessary documentation, and following any special client guidelines where available.
Patient Follow-Up/Patient Statements: With your permission, we approach the patients regarding pending balances that are due after the claim is processed. Statements are sent to the patients with outstanding balance.
